Search

On April 18, the second session of the 2025 Clinical Case Discussion Forum was successfully held at the National Center for Orthopaedics. Jointly organized by Clinical Medical School and Medical Affairs Office, and hosted by the Department of General Surgery, the event centered on the theme “Tracing the Root, Tackling the Rare.” The session attracted over 1,000 participants—including faculty members and medical students from within and outside the hospital—joining both in person and via livestream.

The session, titled “The Non-Indolent Truth in a Critical Case,” was chaired by Professor Fan Youben, Chief Physician of General Surgery. The expert panel featured a multidisciplinary lineup, including Professor Liu Zhiyan (Director, Department of Pathology), Professor Zheng Wei (Chief Physician, Orthopedics), Professor Qiu Zhongling (Chief Physician, Nuclear Medicine), Professor Wang Ren (Chief Physician, Ultrasound Medicine), Associate Professor Wang Yonggang (Associate Chief Physician, Oncology), and Drs. Deng Xianzhao, Guo Bomin, and Ding Zheng (Attending Physicians, General Surgery). Together, the panel conducted an in-depth analysis of a challenging case involving a 49-year-old male patient diagnosed with metastatic papillary thyroid carcinoma complicated by aggressive osseous metastases.
The case discussion was presented by Dr. Tao Xuanbin, a resident physician from the General Surgery Training Program, who provided a detailed report on the patient’s current symptoms, medical history, physical examination findings, and diagnostic test results. The 49-year-old male patient initially sought care for persistent lower back pain lasting over a month. Imaging from an outside facility revealed a lumbar vertebral mass with a pathological fracture at the L3 vertebra. Despite evaluations at multiple hospitals, the primary tumor remained unidentified. Upon admission to Shanghai Sixth People’s Hospital, a multidisciplinary team (MDT) consultation raised suspicion of a thyroid origin. A subsequent PET-CT scan revealed a suspicious nodule at the inferior pole of the right thyroid lobe, multiple pulmonary nodules, and osteolytic destruction at L3 with increased FDG uptake—features highly suggestive of metastatic disease. Thyroid ultrasound and ultrasound-guided biopsy later confirmed multifocal papillary thyroid carcinoma in both lobes. Biopsy of the L3 lesion, together with immunohistochemical analysis and clinical context, supported the diagnosis of dedifferentiated metastatic thyroid carcinoma. The final diagnosis was papillary thyroid carcinoma with pathologic L3 vertebral metastasis and associated fracture. Subsequently, Dr. Zhan Ling, a specialist physician, analyzed the critical role of multidisciplinary collaboration in the diagnostic workflow for thyroid cancer with bone metastases, correlating the discussion with both the case presentation and the patient’s actual clinical circumstances.
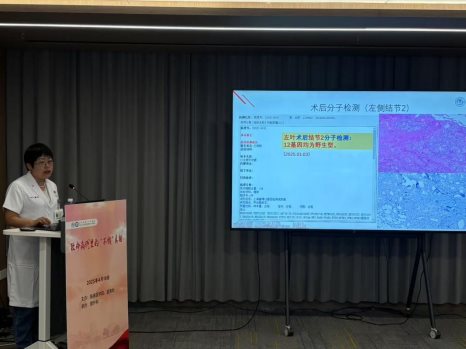
During the discussion session, Dr. Zheng Wei, Chief Physician of Orthopedics, guided resident physicians in an in-depth discussion on metastatic spinal tumors from perspectives such as incidence rate, prognostic and treatment evaluation systems, auxiliary examinations, specialized examinations, and surgical indications. Dr. Liu Zhiyan, Director of Pathology, provided a detailed interpretation of the “temporal and spatial heterogeneity” in postoperative histopathological molecular testing of thyroid cancer, combining preoperative puncture, postoperative pathology, immunohistochemistry, and genetic testing. She emphasized the critical role of pathological quality control. In cases of heterogeneous lesions (where tissue morphology differs from cellular morphology) and when “dominant tumors” are present, molecular testing is recommended based on tumor classification. The genetic alterations in primary and metastatic thyroid cancer lesions are highly consistent. For patients with histopathological evidence of both primary and metastatic
lesions, selection should consider the histomorphological characteristics of both. If different histological manifestations appear, suggesting new molecular abnormalities, molecular testing is advised for poorly differentiated, highly malignant lesions. Dr. Qiu Zhongling, Chief Physician of Nuclear Medicine, analyzed the patient’s nuclear medicine treatment strategy from the perspective of iodine-131 therapy indications and efficacy evaluation. Dr. Wang Ren, Chief Physician of Ultrasound Medicine, shared insights into the ultrasonic imaging characteristics of thyroid cancer and the differential diagnosis of cervical lymph node metastasis. Dr. Wang Yonggang, Associate Chief Physician of Oncology, discussed systemic treatments for advanced thyroid cancer, such as targeted immunotherapy options and prognostic assessments. Attending physician Dr. Deng Xianzhao elaborated on the diagnostic classification, optimal timing for surgery, and the integration of nuclear medicine in managing bone metastases from thyroid cancer. The panel engaged in a dynamic exchange of perspectives. Drs. Ding Zheng and Guo Bomin reported that the patient had successfully undergone both thyroidectomy and spinal surgery without complications, completed a course of iodine-131 therapy, and is now receiving moderate endocrine suppression therapy with favorable recovery. However, due to the severity of the disease, close attention will be paid to comprehensive management and appropriate adjuvant therapy in the follow-up.
Finally, Professor Fan Youben, Chief Physician of General Surgery, concluded the case discussion. He emphasized that this case not only challenged the conventional perception of papillary thyroid carcinoma as an “indolent” disease, but also underscored the importance of active surveillance and timely follow-up for thyroid nodules. He highlighted the pivotal role of multidisciplinary collaboration in the diagnosis and management of complex cases, particularly in rare presentations such as osseous metastasis. This discussion underscored the importance of comprehensive preoperative evaluation, accurate diagnosis, and individualized, standardized treatment protocols. Furthermore, it served as a reminder for clinicians to uphold rigorous clinical reasoning, perform thorough evaluations, and remain diligent in long-term follow-up, all with the goal of delivering optimized care and outcomes for patients.
Latest News
- Tracing the Root, Tackling the Rare: The Fourth Session of the 2025 Clinical Case Discussion Successfully Held11-04
- Intensive Specialized SP Practicum Solidify the Foundation of Clinical Education09-20
- Tracing the Root, Tackling the Rare: Third Session of the 2025 Clinical Case Discussion Successfully Held by Clinical Medical School and Medical Affairs Office08-06
- Tracing the Root, Tackling the Rare: Second Clinical Case Discussion of 2025 Held Successfully07-10
- Tracing the Root, Tackling the Rare: First Clinical Case Discussion of 2025 Held Successfully03-19
- Enhancing Excellence in Residency Training: Specialized Capability Development for Core Faculty12-30
- Supervision Guides a New Journey, Steadfast Actions Ensure Quality Advancement12-06
- Strengthening Residency Training Through Collaboration: 11-20




